A kerfuffle ensued recently when an oncologist and expert on evidence based medicine took the field of cardiology to task over the evidence for placement of the ubiquitous coronary stent. What started with a lengthy article in Propublica that included coronary stenting for stable coronary disease as a prime example of a procedure done without evidence to back it up turned into this fiery twitter exchange between Drs. Kirtane (cardiology) and Prasad (oncology).
The crux of the debate revolves around placement of coronary stents in patients with stable coronary artery disease. Stable coronary artery disease refers to narrowing of the arteries by a build-up of plaque that has occurred slowly over time. Unstable coronary artery disease refers to eruptions that occur within the coronary vessel when a plaque ruptures, quickly leading a patent vessel to become completely occluded or nearly occluded. Unstable coronary artery disease, otherwise referred to as an acute coronary syndrome, is regarded as an emergency that requires urgent intervention by skilled operators (interventional cardiologists) who must race against time to abort a process that if left unchecked may lead to death or severe damage of the heart muscle.
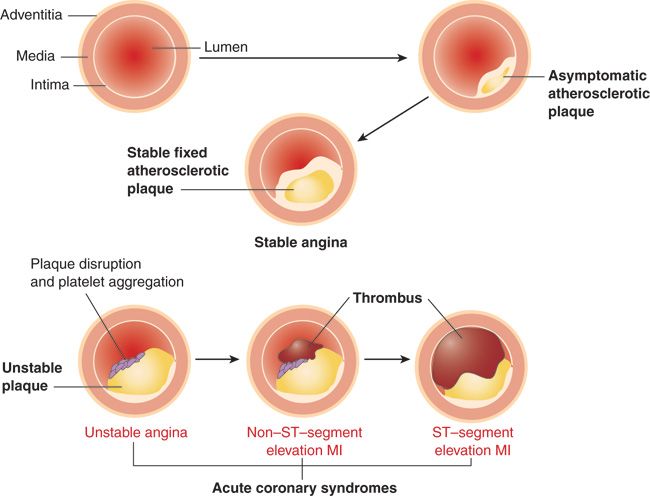
Figure 1. Stable angina/Acute Coronary syndromes
Stable coronary artery disease on the other hand is not considered an emergency, but can result in patients being symptomatic because of diminished blood flow through the culprit artery. Angina pectoris is the descriptor one uses to describe chest pain that relates to a mismatch between the blood flow the heart muscle needs and what it receives. It is almost always the case that angina in stable coronary disease is triggered by activities such as physical or emotional stress that require more blood flow than the narrowed artery can supply.
Patients currently get stents placed for both stable and unstable coronary artery disease, but the debate centers around the evidence for placement of stents in stable coronary disease. Vinay Prasad, an oncologist who apparently spends much time thinking about the heart, believes that there is no data to support placement of stents at all in this setting. The charge is also made implicitly, and explicitly that the only reason for stents being placed in this setting relate to underlying financial incentives rather than the best interest of the patients. Cardiologists, of course, almost universally disagree with these sentiments.
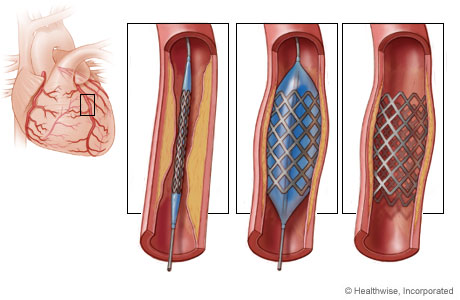
Figure 2. Coronary stent placement
There certainly is blame to be laid at the feet of Cardiologists, but as is usually the case with simple narratives this particular story is not so simple and is deserving of context.
The story of coronary interventions goes back 40 years to 1977. A 37 year old insurance salesman named Adolph Bachmann with severe exercise induced angina had been found to have severe narrowing of a major coronary vessel. At the time the treatment slated would have involved a cardiothoracic surgeon cracking open his chest and bypassing the blockage. Andreas Gruentzig, a cardiologist who had been working on opening up blockages in arteries in the legs by blowing up balloons in narrowed arteries had other ideas. One year earlier Gruentzig had presented the results of his artery opening technique called angioplasty in dogs at the American Heart Association meeting, and had been waiting for the ideal patient to attempt this on. When offered the opportunity to avoid bypass surgery, the insurance salesman enthusiastically leaped at the opportunity. With a cardiothoracic surgeon on standby, Gruentzig guided a catheter across the narrowing, and inflated a balloon across the blockage, proving for the first time in man that a blockage in the heart may be safely treated percutaneously. The patient’s symptoms improved markedly and he remained symptom free almost thirty years after his procedure. The success was not surprising to Gruentzig – the coronary work was simply an extension of his prior work.
By the time Gruentzig attempted this procedure in the coronary artery he had become a master of angioplasty in the larger-diameter vasculature that fed the legs by building on the work of an interventional radiologist named Charles Dotter. Dotter had accidentally recanalized a stenosed iliac artery while doing a routine diagnostic angiography, and understood immediately that the lowly catheter ‘if used with imagination’ could become an ‘important surgical instrument’. Dotter’s first non-accidental patient was an 83 year old woman named Laura Shaw, bedridden for months with a cold, painful left leg admitted for amputation due to progressive gangrene. Deemed too sick for surgery, and with no available options, Dotter proceeded to progressively dilate the artery with successive catheters. The gangrene healed and 83-year-old Mrs. Shaw left the hospital without an amputation – an almost miraculous result at the time.
Gruentzig’s genius was in taking Dotter’s technique and perfecting a balloon catheter to allow for dilation of narrowings, rather than the recanalization Dotter had demonstrated. The first patients he helped were patients like Laura Shaw, with severe disabling pain in the legs from blocked arteries that didn’t allow blood to reach the muscles of the leg. In 1974 – a full three years prior to the first coronary angioplasty, Gruenzig started successfully using his hand made balloon catheter to open up these leg arteries and provide relief to formerly crippled patients.
It was his success in these patients that made Gruentzig so confident about interventions in the coronary arteries. After all, the principle was the same – leg pain was a result of poor blood flow to the muscles of the leg, and chest pain was a result of not enough blood flow to the heart muscle. If relieving blockages in the legs gave function back to patients with leg pain, relieving blockages in vessels of the heart should similarly reduce angina. In Gruenzig’s mind, all that was needed was a smaller catheter and a delivery system to access the coronary tree. He was right.
After his first resounding success, Gruentzig performed four more procedures and published his seminal work as a letter to the editor in Lancet in 1978. The procedure was more successful than anyone could have imagined but still required emergency rescue with coronary artery bypass surgery in 9 of the first 60 cases. Over the next few decades interventions in the coronary vascular tree became safer and easier with ever higher rates of long term success with better techniques and stents to keep narrowed arteries open longer.
Unstable coronary disease, or acute coronary syndromes did not become a focus of cardiologists until a man named Marcus Dewood did what prior had been considered heretical – inject contrast into the coronary artery of a patient having a heart attack. Up to this point no one really understood what happened to patients who had heart attacks. This all changed when Dewood demonstrated it was a blood clot (thrombus) that was completely occluding these important vessels. Cardiologists who had in the past been bystanders to heart attacks as they happened, became active combatants who rushed to open these blocked arteries using the same techniques Gruentzig had pioneered. Averting a heart attack didn’t just relieve chest pain, it prevented death, and heart failure that used to be a natural consequence of heart attacks.
All good things eventually get screwed up, and the same can be said of the field of interventional cardiology. What started in a kitchen with catheters made by hand (Figure 3) became a very big business. And where there is lots of money, nefarious interests seem to intervene. Lots of stents started being placed for a variety of reasons. Cardiac catheterizations were being done not in patients with severe exercise induced angina but in grandpa John with chest pain after his grandson used his sternum as a trampoline. The finding of a narrowing in Grandpa John’s artery should not have warranted a stent, but sometimes did. The impression was left by many cardiologists, either explicitly or implicitly that disaster in the form of a heart attack had been averted.
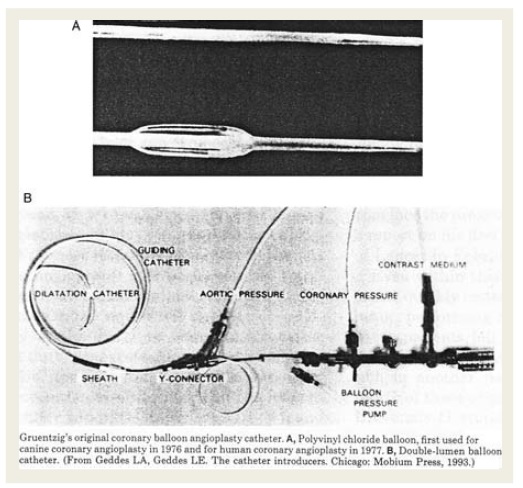
Figure 3. Gruentzig’s original balloon angioplasty catheter
It was visually easy and enticing to fall prey to the idea that opening up nearly blocked arteries was in some way preventing a heart attack. Of course, averting a future coronary event in patients with stable CAD had never been the premise of coronary stents, and the early data that attempted to answer this question suggested the tightest blockages may counterintuitively be the least likely to rupture and cause an acute blockage. Studies at the moment suggest that the likelihood of a plaque rupturing- its stability- is a function of how thick of a fibrous cap overlies it. (Figure 4) Patients with stable CAD who had serial coronary angiograms to study the natural history of coronary plaques appeared to show that the area of highest narrowing, may also be the area that has the thickest fibrous cap.
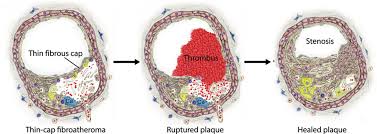
Figure 4. Composition of a coronary plaque
Not surprisingly, studies that randomized patients to medications or stents for stable CAD, showed that patients with stents live no longer. Dealing with the epidemic of unnecessary care prompted guidelines on the appropriate use of stents. Efforts to prosecute and review high volume operators made the national news and sent an especially strong message to the interventional cardiology community. Perhaps as a result, the number of coronary stents for stable CAD fell by 50% from 2009 to 2016.
Critics, however, smelling blood in the water interpret the studies to say that no stents should be placed unless you’re having a heart attack. These are evidence purists who only accept changes in practice supported by randomized controlled trials that preferably show a mortality benefit. They are unimpressed by the effect of stents on angina because the patient is not blind to the intervention. A placebo is a powerful thing – and angina is a subjective complaint. Convincing these puritans requires a control arm that’s a sham – the patient must believe a stent was placed to know if stents have benefit.
Regrettably, what stands in the way of generating perfect data for the apostles are ethical cardiologists who refuse to randomize patients they believe will be harmed by no intervention. Randomizing a patent requires uncertainty on the part of the randomizer – a doctor who believes one arm of a trial may be harmful to his patient cannot be expected to put the trial before his patient. Importantly, primum nocere (do no harm) applies regardless of how wrong the doctor may be proved in some future era. The physician who is out of step with a future he does not know carries no more blame than the Italian mother who refuses to let her son voyage to India by sailing West because she fears he will fall off the edge of a flat earth.
Randomized controlled trials thus fail to apply to patients that were never included in the trial because cardiologists refused to randomize them. The patients excluded in this case are patients with severe disease – those who were unable to be stabilized with medical therapy, or those with disease that jeopardized a large amount of heart muscle. These decisions are not at the fanciful whim of cardiologists but instead are data driven, albeit the non randomized kind. While most significant narrowings may have a thick fibrous cap that makes them stable, not all do. Some highly stenotic plaques in critical areas do rupture, and the consequences of this are severe. To understand what I mean by blockages in critical areas, consider the consequence of an obstruction of the water main that leads to a house versus one that leads to the basement powder room. One makes the house unlivable while the other is a minor nuisance. Navigating a 1% chance of a water main obstruction is all together different than a 1% risk of losing use of a powder room.
The problem with coming down too hard on stents is that the trials to date have specifically excluded patients with ‘water main’ like obstructions. On top of that the whole idea that coronary occlusions/heart attacks evolve from mild lesions may be wrong. The original data on this came from studies that evaluated serial coronary angiograms. This has the small problem of excluding patients who die before they can get their next angiogram. Post mortem studies of subjects dying from cardiac arrest or an acute MI note that the % luminal area of narrowing was >75% in two-thirds of cases, and the mean stenosis of likely culprit lesions causing an MI was 90%.
My intent is not to convince the reader or the purist that overzealous cardiologists may actually have been doing the right thing in their stent orgy, but rather to attach reasonable doubt and fear to doing nothing to the 45 year old father of three who has a water main like obstruction.
In addition, the studies in patients with stable CAD don’t really show that stents are ineffective for angina ( Gruentzig’s original indication ). The most famous study hailed as evidence of the futility of stents – COURAGE – actually reported that one-third of the patients randomized to medical therapy ended up needing a stent. The actual conclusion of the trial was that in stable, low risk patients with angina, an initial strategy of medical therapy was safe and effective and would avoid a stent in two-thirds of patients. This was a worthy conclusion, but a far cry from the conclusion that no stents should be placed for stable coronary artery disease.
I have no doubt skeptics mean well and have patients in mind when they question the motives of cardiologists, but these ad hominem attacks are devastating precisely because of the vast information asymmetry that exists between patients and doctors. Patients simply can’t hope to know as much as cardiologists know about stents. The basis of any argument a physician makes relies heavily on the truthfulness of the person making the argument. Absolutist critics of coronary stents know what they are doing. Having made up their mind about stents from their review of the available randomized control trials, they favor a moratorium on all stent placement outside the realm of those having a heart attack. Since they can’t convince the larger cardiology community of this, their campaign necessarily involves casting doubt on the motives of cardiologists. It’s an understandable but unfortunate approach. It makes for meaty headlines to suggest cardiologists who place stents purposefully ignore evidence to line their pockets – but it would be a gross mischaracterization. I don’t mean to suggest patients should accept their doctors’ assertions about invasive therapies without question. A recent review of a registry of cath labs found 14% of stents placed for stable disease could be inappropriate. This continues to be too high a number, though I wouldn’t focus too much on that absolute number because what is defined as appropriate has a tendency to change from year to year. I do mean to suggest that when it comes to stents in stable coronary disease, don’t throw tomatoes at the next cardiologist who recommends one.